Focus on Maternal Health
Maternal Health Crisis
The United States is the only developed country(leaves FCC.gov, opens PDF file in new browser window) experiencing rising rates of maternal mortality and severe maternal morbidity. In 2022, the infant mortality rate also increased for the first time in two decades. This nationwide crisis impacts Non-Hispanic Black and Native American pregnant women at almost two-to-three times the rate of Non-Hispanic white pregnant women. Furthermore, pregnant women living in rural areas are 60% more likely to die than women living in non-rural areas. Research suggests that many of these deaths, complications, and inequities can be prevented.(leaves FCC.gov, opens new browser window) As Federal Communications Commission (FCC) Chairwoman Jessica Rosenworcel has noted, "It is heartbreaking to see how difficult it is to welcome new additions to families in rural areas without the support needed for a healthy pregnancy. But solutions to this crisis exist and technology can help."
In addition to the increasing maternal deaths and significant and widening disparities in maternal health outcomes:
- The U.S. is facing the increasing prevalence of worsening mental health and substance use disorders among reproductive-age and pregnant women. For example, the number of women with opioid-related diagnoses at delivery increased by 131% between 2010 and 2017.(leaves FCC.gov, opens new browser window) Mental health issues and substance use have been associated with poor maternal health outcomes.
- Women have also started having children later in life, with the mean age of mothers at first birth reaching a record high, at 30 years.(opens PDF file in new browser window) The risk of developing chronic conditions such as hypertension and gestational diabetes during pregnancy increases with age, leading to a higher likelihood of poor maternal health outcomes. Infants born to women with chronic conditions are also at a higher risk of experiencing poor outcomes.
- Access to maternal health care remains a significant challenge, especially for women in rural areas and from lower income households. According to the March of Dimes(leaves FCC.gov, opens PDF file in new browser window), more than 2.3 million women of childbearing age live in "maternity care deserts"—areas where there are no hospitals or birth centers offering obstetric care and no obstetric providers—and an additional 3 million women live in counties with limited access to maternity care.
- Recent data show that over 80% of maternal deaths could be prevented.(leaves FCC.gov, opens PDF file in new browser window) Telehealth and other broadband-enabled solutions and technologies can be a part of the toolkit for improving maternal health and addressing preventable deaths. Prior work by the Connect2HealthFCC Task Force (Task Force) has also shown that populations living in counties that have higher broadband connectivity tend to have better health,(leaves FCC.gov, opens PDF file in new browser window) strongly suggesting that access to and adoption of broadband itself may be related to improvements in health and health outcomes.
Data Mapping to Save Moms' Lives Act
To address these tragic maternal health outcomes, the FCC is playing an increasingly greater role in advancing connected health and improving health care access through telehealth and other advanced broadband-enabled health technologies in the United States. In December 2022, President Biden signed the Data Mapping to Save Moms’ Lives Act (Public Law No 117-247), which directs the FCC to incorporate publicly available data on maternal mortality and severe maternal morbidity into the agency's Mapping Broadband Health in America platform, in consultation with the Centers for Disease Control and Prevention (CDC). Congress aimed to "increase the quality of maternal care and reduce the prevalence of poor maternal health outcomes" by generating maps that provide insight on the intersection of broadband and maternal health “where maternal mortality rates are especially high and . . . where critical telehealth resources need to be deployed.”
Previously, the Mapping Broadband Health in America platform was updated in June 2023 to allow users to view the intersection of broadband connectivity and maternal health outcomes. The 2024 release includes additional maternal health and infant health data that can be leveraged for a variety of questions and decisions. For example, users can:
- Ask questions like, what is the status of Internet connectivity in areas where maternal mortality, severe maternal morbidity, or infant mortality are highest?
- Generate actionable insights for policies and programs about how broadband connectivity can be leveraged to improve maternal and infant health outcomes and identify health disparities.
- Display selected data on broadband connectivity (e.g., fixed and mobile access, Internet adoption, rural access) and maternal health outcomes with key variables to generate customized maps at the state and county levels.
- View maternal mortality, severe maternal morbidity, or infant mortality rates filtered by demographics, social and economic factors, maternal age, race/ethnicity, prenatal care in the first trimester, and rurality to visualize patterns, possible disparity issues, and locations where broadband-enabled interventions may be impactful.
Mapping the Intersection of Broadband and Maternal Health
Given the complexity of the data and compressed timeframe to respond to the Act, the Task Force planned and implemented a multi-phase approach. The Task Force undertook an ongoing consultation with the CDC, relevant agencies within the U.S. Department of Health and Human Services, and other stakeholders to gather their input on the maternal health data and information to incorporate into the mapping platform.
Additionally, the Commission issued a Notice of Inquiry in October 2023 to obtain public comment on ways the Task Force can further expand, refine, and enhance the platform to help better leverage broadband and broadband-enabled health technologies to improve maternal health. Consistent with that objective, the Task Force also pursued proactive efforts to engage key federal agencies and other stakeholders to gather additional input. Furthermore, in November 2023, the Task Force hosted a public roundtable event, titled “The Connected Future of Maternity Care: Intersecting Maternal Health and Broadband Data,” to gather public and private sector thought leaders to explore the intersection between broadband connectivity and maternal health, the role of broadband as a social determinant of health, and the implications of this framework to improve maternal health and health outcomes.
Based on this feedback, the Task Force developed an initial conceptual framework to guide this effort, as described below. Purple diagonal lines denote items from the previous release; blue solid fill denotes the October 2024 release; grey horizontal lines indicate items that will be considered for the future.
What's New? In the 2024 release, a number of new variables relevant to the broadband connectivity and maternal health relationship have been added, including chronic disease (hypertension, diabetes, obesity), smoking during pregnancy, breastfeeding initiation, pre-term birth, low birth weight, prenatal care, infant mortality, digital device ownership, updated broadband access and adoption variables, access to care via transportation, poor mental health days, health insurance coverage by type (e.g., private, Medicaid, Medicare), Veteran prevalence, food insecurity, and social vulnerability.
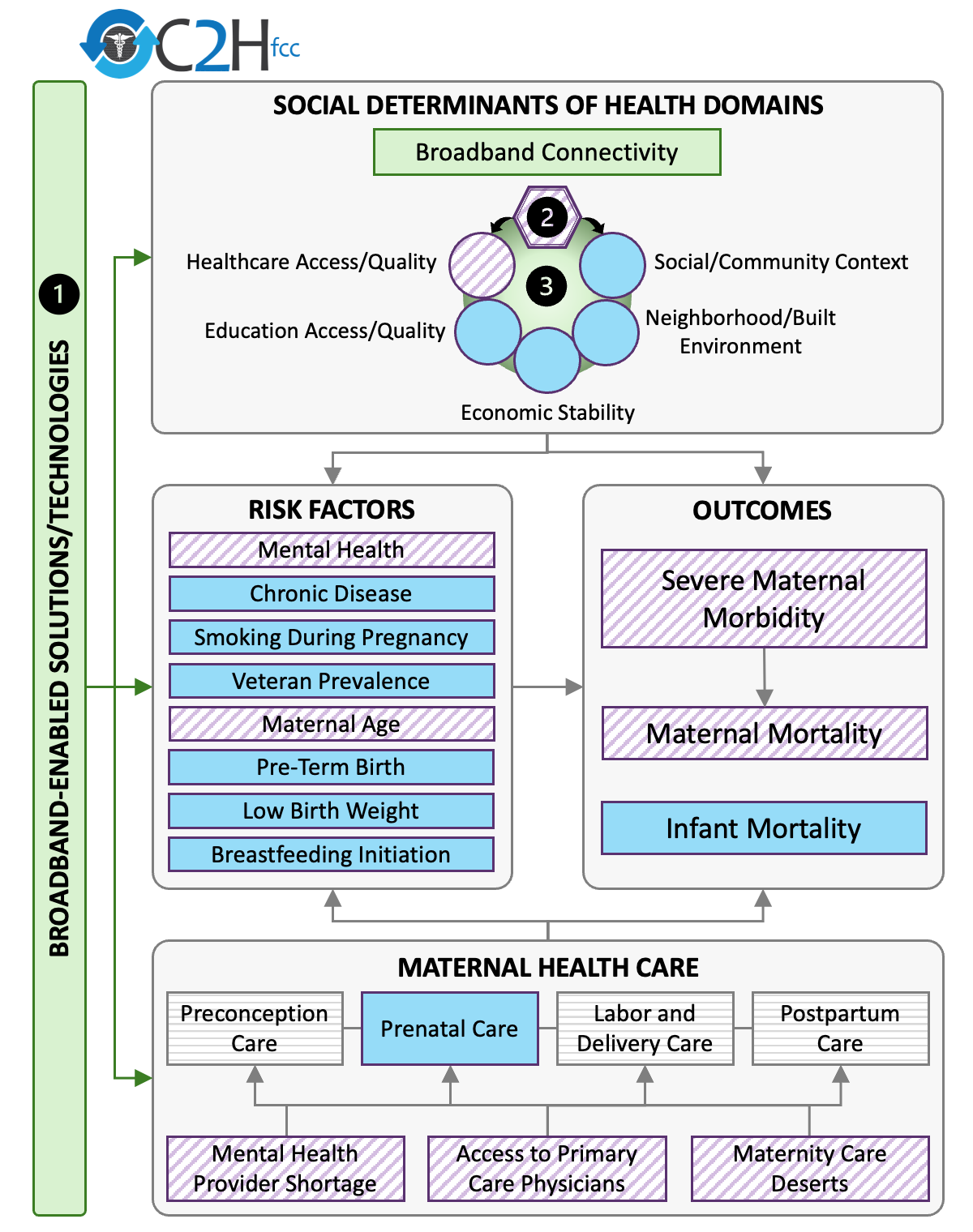
The OUTCOMES box of the framework includes three measures for maternal mortality and one for severe maternal morbidity, including for not less than 1 year postpartum, as directed in the Act. The FCC also recently updated the conceptual framework (as well as the platform) to include infant mortality rate.
- Severe Maternal Morbidity: Not all women who suffer serious and life-threatening complications of pregnancy die from these causes. Instead, many experience “unexpected outcomes of labor and delivery that result in significant short- or long-term consequences,” called severe maternal morbidity. These “near-misses” for maternal death include 20 severe indicators that women can experience during delivery hospitalization, like hysterectomy, ventilation or temporary tracheostomy.
- Maternal Mortality Rate: The World Health Organization defines maternal mortality as “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.”
- Infant Mortality Rate: The CDC defines infant mortality as “number of deaths under age 1 year per 1,000 live births.” Key factors that influence maternal health outcomes, such as access to prenatal care and chronic disease, also impact infant health outcomes including infant mortality.
Much of the data for severe maternal morbidity and maternal mortality outcomes are either unreliable or suppressed at the county level due to low numbers, meaning that those data are only available at the state level. The need for more reliable data on maternal health at the county level has previously been noted in the White House Maternal Blueprint and the Surgeon General’s Call to Action to Improve Maternal Health. The Task Force uses risk factors such as hypertension, gestational diabetes, and obesity as proxy variables, given their availability at the county level and their association with severe maternal morbidity and maternal mortality outcomes.
The SOCIAL DETERMINANTS OF HEALTH box of the diagram includes Broadband Connectivity as an addition to the five social determinants of health (SDOH) domains developed by the Office of Disease Prevention and Health Promotion (ODPHP) Healthy People 2030 program.
- SDOH are “the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.” Examples of SDOH include food insecurity*, health insurance*, poverty,* and rurality.*
The Task Force also identified relevant risk factors that influence maternal health outcomes and where broadband-enabled interventions might help bridge the gaps. The RISK FACTORS box of the framework includes eight measures:
- Mental Health*: Depression affects 1 in 10 women aged 18-44 years of age. Mental health conditions, including suicide, overdose/poisoning related to substance use disorder, are the leading cause of pregnancy-related death.
- Chronic Disease: Chronic conditions like obesity, hypertension, and gestational diabetes can increase the likelihood of poor maternal and infant health outcomes. Maternal obesity is linked to gestational diabetes, hypertension, preeclampsia, preterm delivery, and infant death. Hypertension is one of the most common pregnancy complications and a leading cause of pregnancy-related death, and with higher rates for Black women and American Indian/Alaskan Native women as well as women over 35.
- Smoking during Pregnancy: Smoking during pregnancy can lead to low birth weight, pre-term birth, stillbirth, birth defects, sudden infant death syndrome (SIDS) and abnormal maternal bleeding. It can also cause fertility problems for future pregnancies.
- Veteran Prevalence*: Pregnant Veterans are more likely to have poor maternal health and mental outcomes in comparison to civilian women. Military service adds unique risks, including sexual trauma, injuries, mental health issues, and environmental exposures, further increasing the risk of poor pregnancy outcomes, like preterm birth.
- Maternal Age: Increased age during pregnancy is associated with a greater risk of obstetrical complications, and maternal mortality rates are 6.8 times higher for women over 40 years old compared to women under 25.
- Pre-Term Birth: Pre-term birth affects approximately 1 in 10 infants in the United States and is a leading cause of infant mortality. Women over 35, those with lower incomes, and Black, Native Hawaiian, Pacific Islander, American Indian, or Alaska Native women face a higher risk of pre-term birth.
- Low Birth Weight: Low birth weight affects about 1 in 12 infants in the United States and is a leading cause of infant mortality. The primary causes are preterm birth and fetal growth restrictions. Risk factors for having a low birth weight baby include smoking, alcohol consumption, infections, chronic conditions, and being over 35 years of age.
- Breastfeeding Initiation: For infants, breastfeeding is associated with lower rates of asthma, diabetes, obesity, cancer, and SIDS. For mothers, breastfeeding is associated with lower risk of Type 2 diabetes, breast, and ovarian cancer. Breastfeeding rates are lower for Black, Native Hawaiian, Pacific Islander, American Indian, or Alaska Native women. There are also significant connections between breastfeeding and maternal mental health outcomes.
The MATERNAL HEALTH ACCESS box of the framework includes four indicators:
- Maternity Care Deserts: Areas with no maternal care resources, which may also have lower access to broadband services. Some researchers estimate that 70% of counties with the highest proportion of low-speed Internet providers did not have full access to maternity care.
- Mental Health Provider Shortage Areas*: Areas with limited mental health providers and resources. Maternal mental health conditions affect 1 in 5 women during or after pregnancy, and are one of the most common causes of pregnancy-related deaths (22.7%). Broadband connection can enable digital capabilities such as navigating care, identifying risks, building community, and connecting to counseling as needed. Telehealth services can help connect patients and mental health providers.
- Access to Primary Care Providers*: Primary care providers often serve as obstetric providers, especially in rural areas, before, during, and after pregnancy. This is due to an obstetric care workforce shortage across the country.
- Prenatal Care: Babies without prenatal care are three times more likely to have a low birth weight and five times more likely to experience infant mortality.
Information on the data sources utilized for Broadband Connectivity, SDOH, Risk Factors, Maternal Health Care, and Maternal and Infant Health Outcome can be found on the Data page.
*The data on these variables pertain to the general population and do not specifically focus on pregnant or postpartum individuals.
Future Work
The Mapping Broadband Health in America platform is a foundational tool for understanding the intersection of broadband and health, giving policymakers, researchers, advocacy groups, health care providers, and other interested parties a concrete path to a more connected and healthier future for all Americans.
Broadband connectivity is showing promise as an integral resource to help improve maternal health outcomes, including:
- Acting as a distinct social determinant of health, which could help to improve health equity and close the digital divide.
- Providing an innovative means to deliver maternal health solutions and health care.
- Connecting users with the resources they need to get healthy or stay well.
- Enabling activities that are associated with better health such as employment and education.
- Mediating the ways in which the other established social determinants influence health and is, therefore, considered a “super” determinant of health.
The Task Force will continue to refine the conceptual approach going forward and welcomes comments and suggestions from interested parties via e-mail to engageC2H@fcc.gov(opens email application with "Mapping" in the subject line).