Focus on Broadband and Opioids
The opioid crisis has been ravaging communities and families across the United States for the past decade. In 2017, the opioid crisis was declared a public health emergency under section 319 of the Public Health Service Act, and that declaration was renewed most recently in June 2024 (opens new window). This crisis claims more than 220 lives per day (opens new window). Evidence also suggests that the impacts of the opioid crisis have been exacerbated during the COVID-19 public health emergency with significant increases in alcohol and substance misuse and worsening mental health. Recent research, however, suggests that the use of telehealth services and medications for Opioid Use Disorder was associated with reduced risk for fatal overdoses (opens new window) during the COVID-19 pandemic, and telehealth was associated with an increased likelihood of staying in treatment for opioid use disorder (opens new window), indicating that broadband-enabled solutions may provide critical tools in addressing the challenge.
According to the Centers for Disease Control and Prevention:
- More than 645,000 people (opens new window) in the United States have died from overdoses involving opioids since the epidemic began;
- The number of annual opioid overdose deaths remains more than six times higher (opens new window) than it was in 1999;
- There were approximately 81,806 opioid overdose deaths in 2022 (opens new window) and 90% involved synthetic opioids other than methadone; and
- Provisional data reflects that the number of drug overdose deaths began to decrease in 2023 (opens new window), the first time since 2018, and provisional 2024 data from the CDC indicates a further decline in drug overdose deaths (opens new window), although much work remains.
Of course, opioid overdoses may also be non-fatal. These non-fatal opioid overdoses place significant burdens on governments, health systems, communities, and families and may disproportionally affect rural and underserved areas. For example:
- There were nearly 290,000 hospitalizations and emergency department visits (opens new window) related to opioid poisoning in 2016.
- Most of these hospitalizations and emergency visits were paid for by Medicare, Medicaid, or the uninsured (opens new window).
- Rural counties may experience resource shortages or limited economic opportunities that negatively affect access to health care services and health outcomes.
In recognition of the potential of broadband to help stakeholders respond to this crisis, particularly in rural areas, Congress directed the Federal Communications Commission to update its Mapping Broadband Health in America platform to include data on drug misuse. In response, the Connect2HealthFCC Task Force launched a novel analytic and consultative process to determine how best to intersect broadband and drug misuse data in ways that would draw meaning from the data and lead to actionable intelligence for policymakers and other stakeholders. For instance, policymakers can examine which counties have both low Internet adoption and high Opioid Use Disorder prevalence along with shortages in mental health services to identify areas that could benefit from increased access to telemental health services. We used an evidence-based approach to conceptualize the intersection between drug and opioid misuse and connectivity, with a particular focus on identifying areas where broadband-enabled interventions could make a difference in access to care or health outcomes.
Multi-phase effort
The integration of drug misuse data into the Mapping Broadband Health in America platform is a multi-phase project and the most recent refinements reflect thoughtful review of the broadband and opioid landscape, as well as input and feedback from key stakeholders and users.
What’s new? In the October 2024 release, a number of new variables relevant to the broadband connectivity and opioid misuse relationship have been added, including digital device ownership, updated broadband access and adoption variables, access to care via transportation, poor mental health days, health insurance coverage by type (e.g., private, Medicaid, Medicare), Opioid Use Disorder prevalence, Veteran prevalence, race and ethnicity, food insecurity, social vulnerability, and HIV prevalence.
The platform - which is available at www.fcc.gov/health/maps (opens new window) - allows users to identify and characterize the specific broadband/opioid challenges at the local level, point to solutions, and spark collaborations. Specifically:
- Users can ask questions like, what is the status of Internet connectivity in areas where the opioid crisis is being driven by higher prescription rates (i.e., there may be a need to augment prescription drug monitoring programs and connectivity for health) vs. illicit drug use.
- Users can display selected data on opioid mortality and prescription rates from the CDC with the fixed broadband deployment data from the FCC to generate customized maps at the national, state, and county levels that explore the intersection between drug misuse and Internet connectivity. In addition to fixed broadband access, the platform visualizes metrics on Internet adoption, rural broadband access, and device ownership in a selected geographic area.
- Percent change in opioid mortality and prescription rates enable users to visualize trends and identify potential emerging “hotspots” of the crisis, where broadband-enabled interventions might prove fruitful.
- Opioid mortality rates and trends have been broken down into several categories that reflect shifts in the primary type of opioid driving the crisis as it has evolved.
- Risk factors affecting opioid misuse and overdose have been added, including poor mental health days and access to healthcare (such as transportation, mental health provider shortages, and health insurance coverage).
- Opioid Use Disorder prevalence, a key health outcome variable, has been added.
- Users can also filter by rurality and overlay other key community factors (such as race and ethnicity, and veteran status), and important economic indicators (including poverty, food insecurity, and the social vulnerability index) to better understand the intersection between drug misuse and broadband.
- One ongoing challenge is the reality that community-level data are not available for all relevant data points; we hope to further tackle those pre-existing data gaps in later refinements.
| Drug misuse variable | Description |
|---|---|
| All drugs | Deaths and trends due to all drug overdoses for any reason (unintentional, suicide, homicide, or undetermined). |
| Any opioid | Deaths and trends due to overdoses for any reasons and involving opium, heroin, natural and semi-synthetic opioids, methadone, synthetic opioids other than methadone, and other and unspecified narcotics. |
| Prescription opioids | Deaths and trends due to overdoses for any reason and involving natural and semi-synthetic opioids and methadone. |
| Synthetic opioids | Deaths and trends due to overdoses for any reason and involving synthetic opioids other than methadone. |
| Heroin | Deaths and trends due to overdoses for any reason and involving heroin. |
| Opioid prescriptions | Prescriptions include any initial or refill prescription dispensed at a retail pharmacy in the sample and paid for by commercial insurance, Medicare, Medicaid, cash or its equivalent. Opioids include, but are not limited to, buprenorphine, codeine, fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxycodone, oxymorphone, propoxyphene, tapentadol, and tramadol. |
| Opioid use disorder | Prevalence of overarching Opioid Use Disorder (OUD) among Medicare (dual and non-dual) beneficiaries. |
Broadband and Opioids Conceptual Model
To determine how best to intersect connectivity and opioids data, the Task Force began by reviewing the available literature on opioids and connected health. The goal was to inform a conceptual model for intersecting broadband and drug misuse data. Specifically, we identified key evidence-based factors that were important to better understand and address opioid use disorder, overdose, and mortality at a population level - forming a potential roadmap for leveraging broadband telehealth, and other advanced broadband-enabled health technologies as part of the overall solution. These factors and their relationships are presented in the resulting Conceptual Model that underlies the current mapping platform. (Read more about our methodology here.)
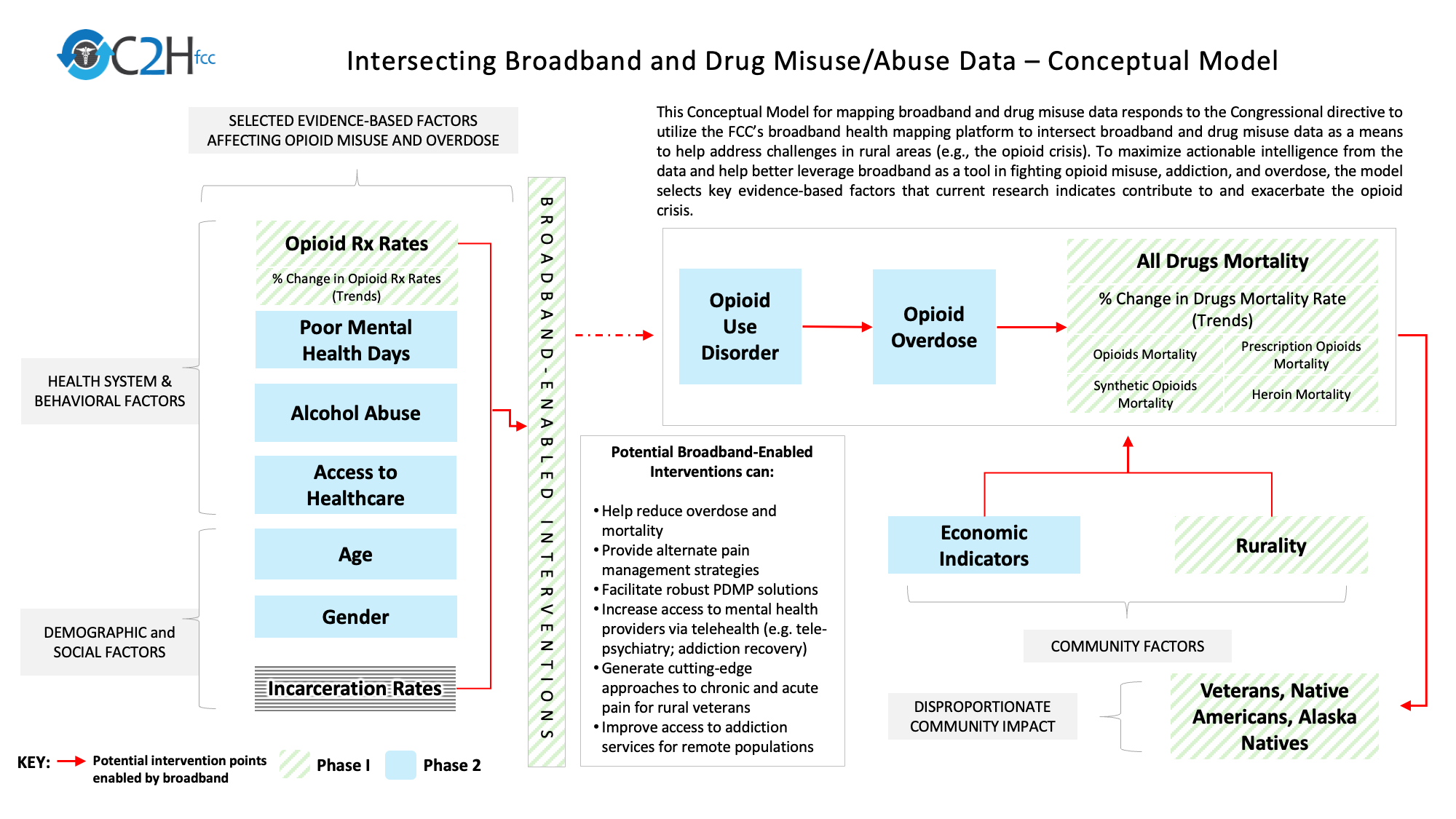
- Opioid prescription (Rx) rates provide information on the number of prescriptions in a community that may indicate availability and exposure to opioids.
- Poor mental health days reflect the burden of disabilities and chronic diseases as well as health-related quality of life among individuals living in a community.
- Alcohol and other substance misuse may create an environment that enables opioid misuse and overdose.
- Access to mental health providers provides information on the availability of services for individuals to both seek preventive care and receive treatment for opioid misuse.
- Access to healthcare, including access to primary care providers, access to transportation, and having health insurance decreases risk of Opioid Use Disorder.
- Demographic and social factors, such as age, gender, income, food insecurity, education, unemployment, and incarceration rates, may account for important differences in prescribing, use, and misuse of opioids that exists in a community.
- Community factors, such as economic indicators and rurality, may also account for important differences in access to care and treatment.
- Population groups such as veterans, Native Americans, and Alaska Natives may also experience a disproportional community impact from the opioid crisis.
- Opioid-related outcomes, such as increased incidence of blood-borne infections such as HIV.
The Conceptual Model also recognizes the evolving nature of the opioid crisis. The CDC characterizes the crisis in three distinct waves identified by the primary type of opioid driving the spike in overdose and mortality.
- Wave 1 (1990s): The crisis began in the 1990s with a first wave of deaths due to a rise in overdoses involving prescription opioids, including natural and semi-synthetic opioids and methadone.
- Wave 2 (2010 - 2013): This was followed by a second wave in 2010 with a spike in heroine-involved deaths.
- Wave 3 (2013 - present): The present wave is defined by a rapid increase in deaths due to synthetic opioids other than methadone (opens new window) (including fentanyl, fentanyl analogs, and tramadol) since 2013. Between 2021 and 2022, synthetic opioid deaths increased by 4% (opens new window) and now account for about 90% of opioid-involved deaths.
Potential of Broadband in Addressing the Opioid Crisis
Finally, the Conceptual Model integrates the potential of broadband as a powerful resource that may be leveraged to combat the opioid crisis, helping to save and improve lives in the U.S. For example, various studies (opens new window) have shown that use of telehealth can greatly improve access to and delivery of behavioral health services, including those for substance use disorders, but this full potential has not yet been realized. In addition, broadband-enabled interventions could potentially:
- Help to reduce overdose and mortality related to drugs and opioids;
- Support innovative pain management strategies;
- Facilitate robust, digital solutions for Prescription Drug Monitoring Programs;
- Increase access to mental health providers via telehealth (e.g., telepsychiatry, addiction recovery); and
- Generate cutting-edge approaches to chronic and acute pain for veterans.
We will continue to refine the conceptual approach going forward and welcome comments from interested stakeholders via email to engagec2h@fcc.gov.